The Respiratory System
All right, so we’re going to run through the respiratory system in this article. Before we get into the anatomy, let’s go over the basic functions.
The respiratory system supplies the body with oxygen and disposes of carbon dioxide. There are four processes involved with respiration.
- Pulmonary ventilation is the air being moved in and out of the lungs.
- External respiration is the gas exchange in the alveoli.
- Transport of respiratory gases occurs via the cardiovascular system.
- Internal respiration is the gas exchange that occurs at the capillaries and intercellular tissues.
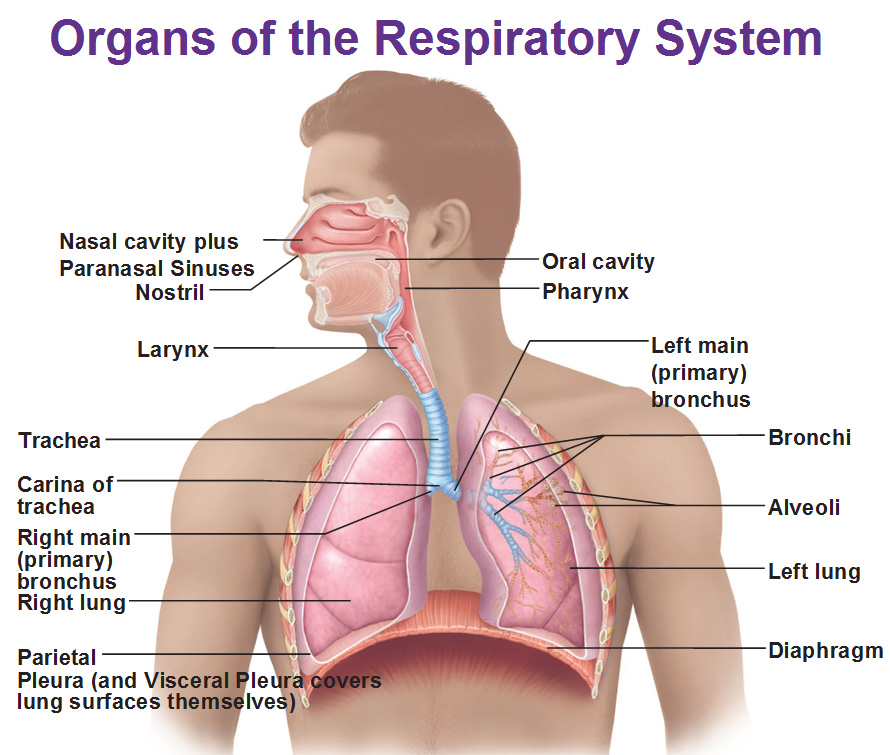
The organs of the respiratory system are divided into the conducting zone and respiratory zone. The conductive zone carries, filters, humidifies and warms incoming air. The respiratory zone is the site where the actual gas exchange occurs. We will start with the conductive zone and then as things get smaller, we will eventually hit the respiratory zone.
Structures of the Conductive Zone
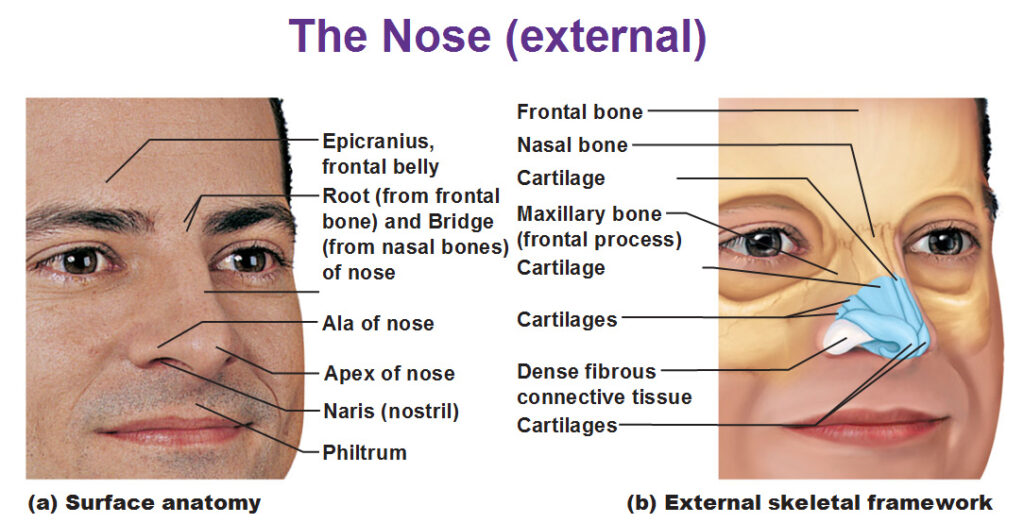
Okay so here’s our guy above. On the right is our nose structure to show what’s inside our skin. You already know the frontal bone with the epicranius that sits on top of it. There’s a nasal bone split into two that is going to make the bridge of your nose. Fill these bones with cartilage and you have yourself a nose. The tip/point of your nose has an official name called the apex of nose. In between your nose and your lips is the philtrum while the ala is that section that flares out. Okay, moving on…
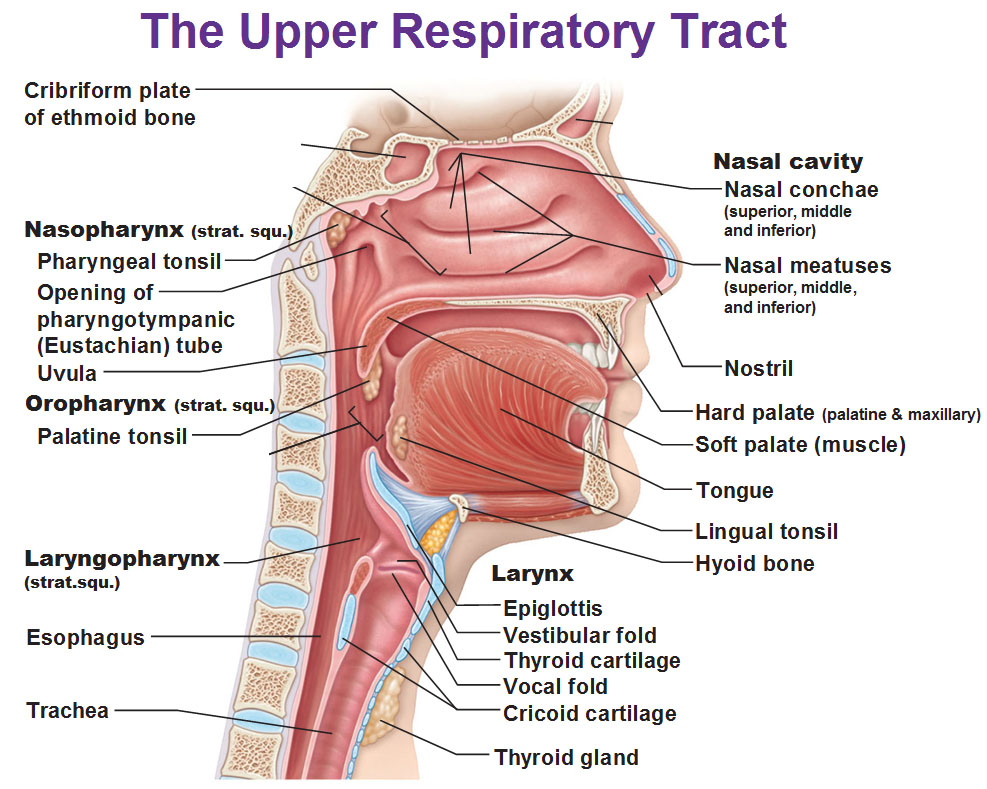
Anatomy of Upper Respiratory Tract (above): Air is going to come into the nasal cavity and pass through the nasal conchae which is covered in mucosa. We’re going to produce mucous in there to trap things like dust or bacteria to prevent them from getting in any further. We would normally have divided this in half with the nasal septum but in this particular view they have removed the nasal septum and we’re looking at the left side of the nose from the right. The pharynx is long and divided into 3 parts. The part that’s behind the nose is called the nasopharynx. The part behind the mouth is the oropharynx. The part behind the larynx is the laryngopharynx. If we continue down there we have the esophagus. If we go in front of the pharynx we have the larynx where we have vocal cords in there. In the larynx is where you see the epiglottis at the top and trachea below it.
Olfactory and respiratory mucosae of nasal cavity
The olfactory musoca are located in the roof of the nasal cavity. The respiratory mucosa are located in the rest of the nasal cavity that are made up of pseudostratified ciliated columnar epithelium with goblet cells (this is what produces the mucus). The cilia up here in the nasal cavity are sweeping down in the direction of the pharynx. You would imagine it’s going to try to stroke it outward the way you blow your nose out but instead it tries to push it in toward the pharynx to be destroyed in the stomach. Underneath this mucosa is a lamina propia with tubuloalveolar glands that contain mucous and serous cells. The mucous contains lysozymes which destroy bacteria. Up to a quart of mucous is produced per day.
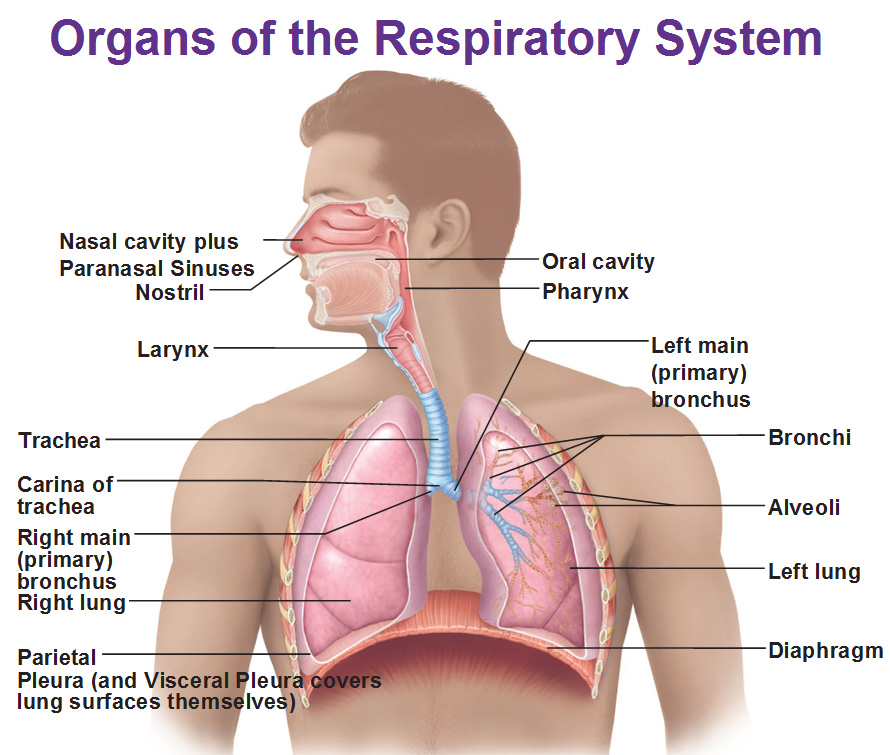
Larynx (Voice Box)
 This is our voice box. The larynx is made of 9 specially shaped cartilages that are connected by ligaments. Let’s start with the hyoid bone. On top of it are some of the muscles of the tongue. Going below the hyoid bone we find a large cartilage in the front called the thyroid cartilage. This is what sticks out more in men than the ladies. The official name for the Adam’s apple is the laryngeal prominence. Below that we have another piece of cartilage called the cricoid cartilage. Below that is the trachea which we will get into later.
This is our voice box. The larynx is made of 9 specially shaped cartilages that are connected by ligaments. Let’s start with the hyoid bone. On top of it are some of the muscles of the tongue. Going below the hyoid bone we find a large cartilage in the front called the thyroid cartilage. This is what sticks out more in men than the ladies. The official name for the Adam’s apple is the laryngeal prominence. Below that we have another piece of cartilage called the cricoid cartilage. Below that is the trachea which we will get into later.
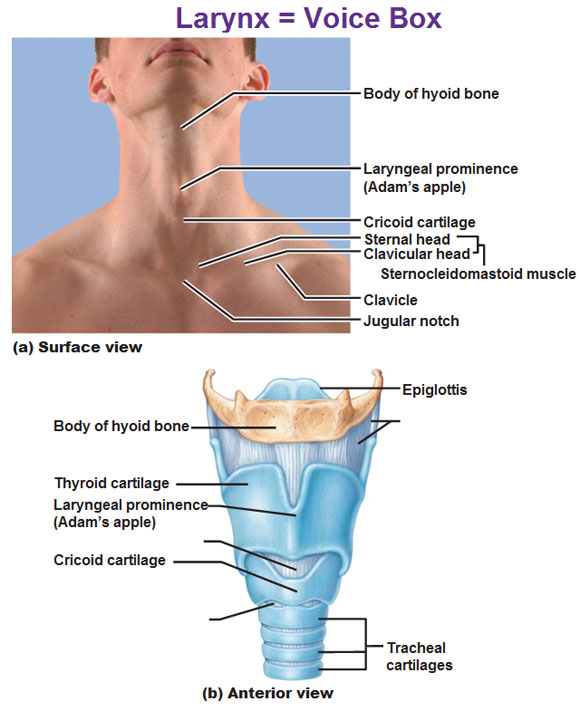
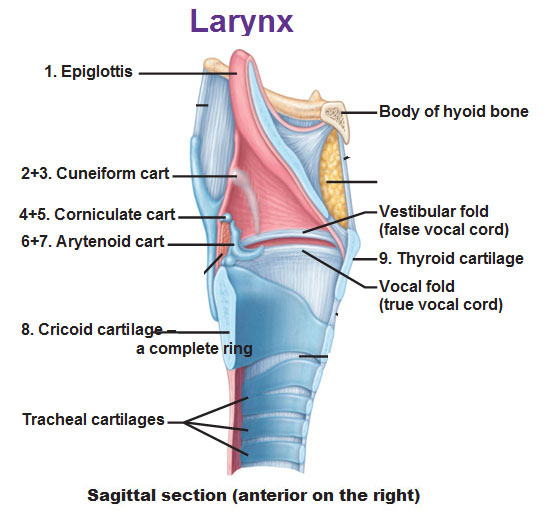 Above is a side view. Here you could see the front part of the thyroid cartilage. The cricoid cartilage is actually a complete ring. The epiglottis is like a flap that sticks diagonally upwards, anchored in the front by the thyroid cartilage and the upper part is sort of free. And we’re going to have a bunch of other little cartilages which are all movable and remember we’re only seeing one half. The cuneiform cartilage is actually two pieces on each side and cuneiform means wedge shaped. Corniculate cartilage has a horn shape, with that root word corn or corny. And we also see the arytenoid cartilage. Arytenoid means cup like or ladle like shape, and it does look that way.
Above is a side view. Here you could see the front part of the thyroid cartilage. The cricoid cartilage is actually a complete ring. The epiglottis is like a flap that sticks diagonally upwards, anchored in the front by the thyroid cartilage and the upper part is sort of free. And we’re going to have a bunch of other little cartilages which are all movable and remember we’re only seeing one half. The cuneiform cartilage is actually two pieces on each side and cuneiform means wedge shaped. Corniculate cartilage has a horn shape, with that root word corn or corny. And we also see the arytenoid cartilage. Arytenoid means cup like or ladle like shape, and it does look that way.
Movement of the epiglottis
The epiglottis is elastic cartilage covered with mucosa that tips inferiorly during swallowing when the larynx moves superiorly, closing off the larynx to keep food out of the respiratory system. So in other words, when you swallow, whether it’s mucous or food, remember we have the pharynx and esophagus behind this larynx, so what happens is the front part of the epiglottis is going to get pushed upward, causing the epiglottis to flop down and cover the opening to the trachea. Right now you could touch your Adam’s apple, swallow, and you will feel your Adam’s apple dramatically rise up for a moment.
True Vocal Cords ( aka Folds or Ligaments)
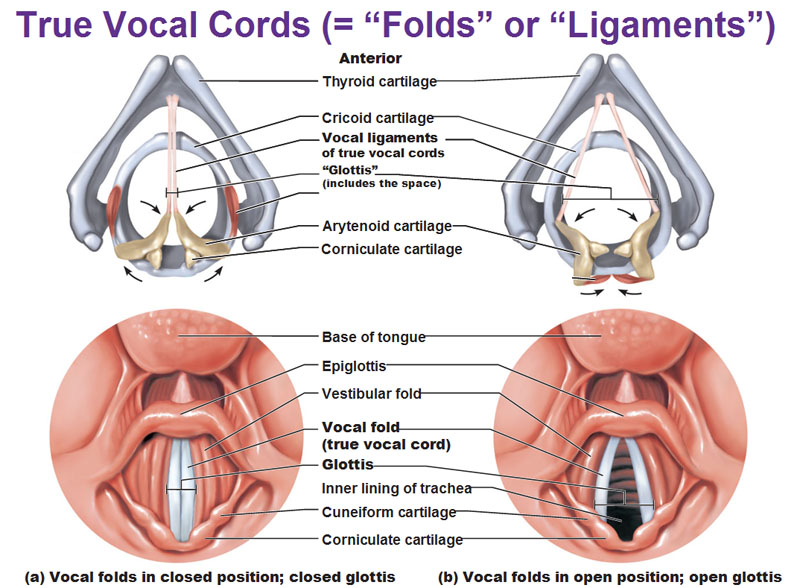
In regards to the picture below: What we’re looking at here is if you’re on top and looking down at the larynx as if a doctor was looking down, waaay far down. What’d they see is all the mucosa covering the structures, but let’s investigate the internal structures to see how this is all put together.
The pointy part is the front. There’s our cricoid cartilage, which is inferior to the thyroid cartilage. Look at these little pink slips in the middle: These are little vocal ligaments that are very elastic and these are your actual vocal cords. They aim anteriorly to attach to the thyroid cartilage. The glottis is the space taken up by the vocal cords, including the empty space when they are far apart.
Top Left annd Top Right photos for above: When you see the arytenoid cartilage is in this position , the vocal cords are very close together but when they are apart, look how far they move on the right side. There are little muscles attached to the arytenoid cartilage that moves them. So if you tug on the posterior portion of the carytenoid cartilage putting them together, the vocal ligaments move apart. This is to allow a lot of air through, which is what sound is made of. A lot of your voice production is from changing the length, positioning, tension of the cords, very much the same way you would tune a string instrument like a violin or cello. You could tighten the strings and change the pitch. You don’t have knobs to turn, instead you have little cartilages that move and these muscles that can move them in very subtle ways. So that is your basic structure.
Bottom Left and Bottom Right photos for above: If we overlay a bunch of mucosa all over this cartilage structure, we get this structure that looks like… well.. looks like a vagina doesn’t? The true vocal cords/vocal folds are white. The vocal ligaments are covered in avascular mucosal tissue meaning they don’t have blood vessels and that’s why they are illustrated in white. The rest of the area is well vasculated so that’s why that’s pink. Immediately lateral to those cords are these vestibular folds which are also known as the false vocal cords (no idea why they have that name to confuse the matter more, vestibular folds was good enough). Its just a fold of extra mucosa, and while it doesn’t function in the way the vocal cords do in the production of sound and sound waves, you do get some functions that modulate the sounds and there’s also an additional function: to help completely seal the airway on purpose. For example, there’s this thing you could do called a valsalva maneuver, like when you’re straining to poop, if you close the airway from the top, it helps seal the opening at the top, so it increases the intraabdominal and intrathoracic pressure on the inside. Because think about it when you’re constipated and you’re pushing, you’re holding your breath, right? That’s the valsalva maneuvar and the vestibular folds (innervated by vagus nerve) are what help fully seal that area.
The larynx – Voice Production
Some of this we’ve talked about before but let’s go over it again. Stratified squamous epithelium is in the top of part of the larynx, including the vocal cord ligaments. Why would this cell structure be a good choice? Mainly for protection because there’s several layers. Whenever you see stratified squamous epithelium, that’s an area where for some reason, you need extra protection from outside (like your skin). If we look at your location of the larynx again, it’s at the top of the airway so if we had a bunch of dust and some cells got sloughed off that would still be okay because there’s a lot of layers.
The inferior half to 2/3rds of the larynx switches to pseudostratified ciliated columnar epithelium (with some cilia, of course) that desperately pushes things up and over into the pharynx. Remember the cilia in the nasal cavity pushes down toward the pharnyx while the cilia in the larynx pushes UP to get stuff into the pharynx to then go in the stomach.
Voice production details: The vibration and clapping together of the cords when air is exhaled past causes sounds. Remember the mucosa over the vocal cord ligaments is avascular. Several tiny laryngeal muscles move arytenoid cartilages to adjust length, position, and tension of vocal folds to change pitch.
During puberty, testosterone is a hormone that is released in a much higher amount in a boy and that causes a lot of changes such as the thyroid cartilage growing much longer than in a girl. If you have a longer thyroid cartilage (look at pic) it will end up in a longer cord which is going to give you a deeper voice because the longer cords vibrate more slowly than shorter cords. So in general, men have deeper voices than women because of this lengthened thyroid cartilage.
The Trachea
This is our next level down from the larynx, made up of 16-20 C-shaped hyaline cartilage rings. In between them we are going to have fibroelastic connective tissue (which is great for breathing cause we wanna expand a bit). These cartilage rings prevent collapse so that you don’t have to re-inflate this tube on top of having to take a breath, so you’re always able to breathe easily.
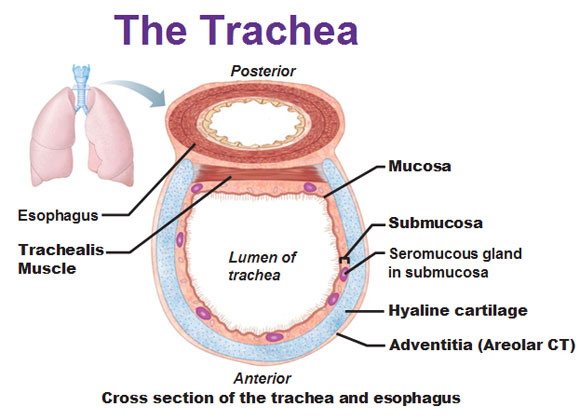 So here we go. Keep in mind the ring is not a full circle, it’s like a horse-shoe shape. In the posterior part where it’s incomplete we’re going to put a muscle right there. That’s a trachealis muscle which is a smooth muscle and when you cough or sneeze this muscle contracts rapidly to really accelerate that air to 100mph, to try to get whatever is bothering you, out of your body. So coughing and sneezing is really a protective mechanism. Of course we have a mucosa layer lining this pseudostratified ciliated epithelium where the cilia sweep upwards. At the carina of the trachea (the very bottom of the trachea, where the trachea splits) the mucosa is extra sensitive to irritants and often triggers the cough reflex.
So here we go. Keep in mind the ring is not a full circle, it’s like a horse-shoe shape. In the posterior part where it’s incomplete we’re going to put a muscle right there. That’s a trachealis muscle which is a smooth muscle and when you cough or sneeze this muscle contracts rapidly to really accelerate that air to 100mph, to try to get whatever is bothering you, out of your body. So coughing and sneezing is really a protective mechanism. Of course we have a mucosa layer lining this pseudostratified ciliated epithelium where the cilia sweep upwards. At the carina of the trachea (the very bottom of the trachea, where the trachea splits) the mucosa is extra sensitive to irritants and often triggers the cough reflex.
In the nasal cavity, the cilia pushes down toward the larynx and below the level of the larynx, you’re going down into the lungs, you want to push everything up so it doesn’t go into your lungs, up and over the top One of the specific mechanisms that are damaged from smoking is the damage to this cilia. That’s why smokers are more prone to getting colds or pneumonia cause things just sort of hang out in the lungs instead of getting pushed out.
Lobes of Lungs and Bronchi
So this structure is our bronchial tree, and it branches, branches, branches, smaller, smaller, smaller that fill up the lung. Bronchi branch to become bronchioles.
The right lung has three sections to it; 3 lobes. The left lung has two sections; 2 lobes. You see there’s a cut out for the heart.
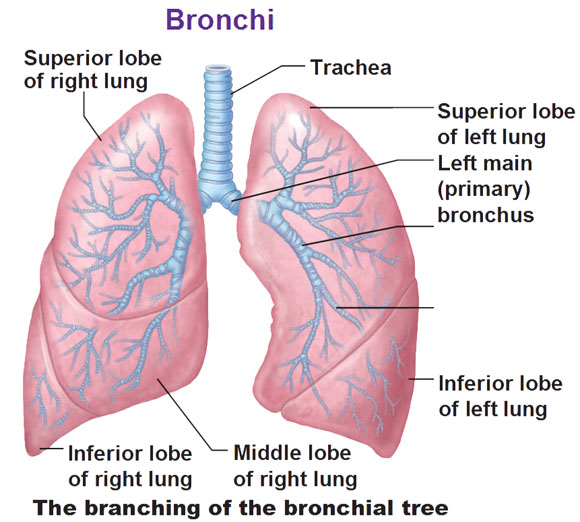
Tissue composition changes along the bronchi
The composition of the tissue is going to change as we go from big tubes to smaller and smaller branches.
First we start with cartilage rings, then they don’t go so far around and they’re called cartilage plates then there’s not gonna be anymore cartilage.
As for the cell type, we start off with…
Ciliated peudostratified columnar on the top then
Ciliated simple columnar,
Ciliated simple cuboidal,
Simple cuboidal (no more cilia nor mucous-producing goblet cells)
The trachialis smooth muscle changes from only a posterior location to an encircling location and thins out at the terminal bronchioles. Smooth muscle is controlled by the autonomic nervous system: so of course a nerve from the parasympathetic and sympathetic system is going to innervate it to create a different effect.
When you’re gearing up for fight or flight (sympathetic shit) what are you going to need in terms of oxygen? LOTS OF IT. So the airways widen. The adrenal medulla releases epinephrine and norepinephrine which are smooth muscle relaxants. so the smaller branches are going to widen.
Under the parasympathetic stimulation, the ACh is released which constricts the airways in case you don’t need so much air (rest and digest).
Structures of the Respiratory Zone
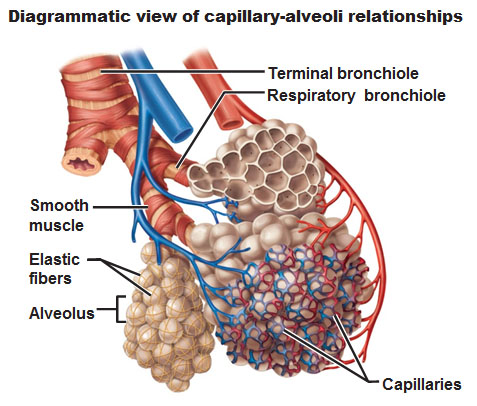
Now we’re getting to the smallest branches of the bronchi, the terminal bronchioles. This is the end of the conducting zone (remember the conducting zone is just the transport of air, not an exchange). Now we continue into the next zone into the respiratory zone because we actually now start to exchange the actual gases. Note that the respiratory bronchioles and everything distal to it are microscopic structures.
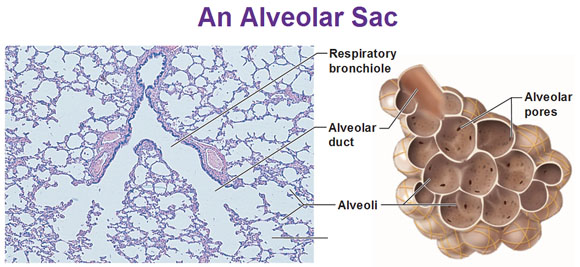
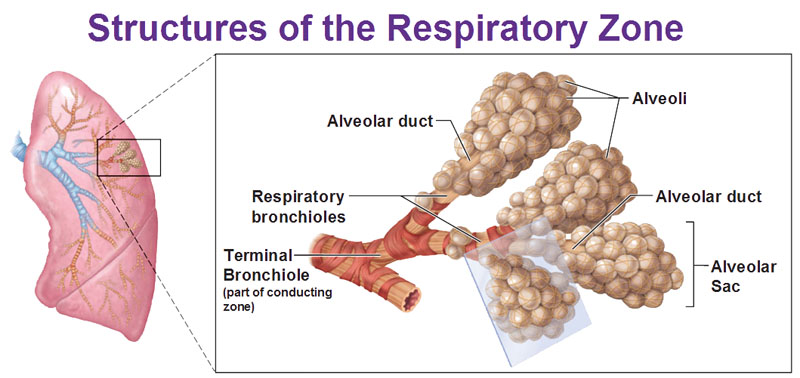 Now you could see smooth muscle wrapping around. At the ends of the respiratory bronchioles we have these alveoli and a cluster of them is the alveolar sac. The alveolar duct is the name of the next branch after the bronchioles.
Now you could see smooth muscle wrapping around. At the ends of the respiratory bronchioles we have these alveoli and a cluster of them is the alveolar sac. The alveolar duct is the name of the next branch after the bronchioles.
As we move into this microscopic level, if we had kept columnar cells, it would take too long for oxygen to diffuse. So that is why we have squamous epithelia present, but it transitions from columnar to cuboidal to squamous. There’s 300 million of these individual alveoli:
The following pictures shows how these capillaries wrap around each of these alveoli so they could reach the oxygen:
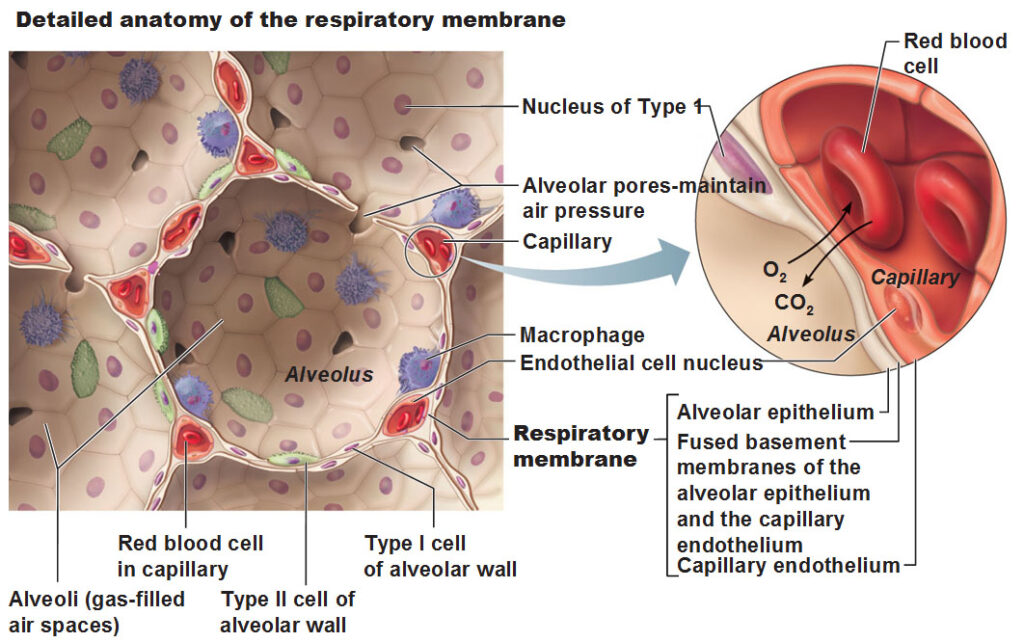
The Respiratory Membrane
Each of these balloons, are made of simple squamous epithelial cells. These particular squamous cells labeled are going to be called Type 1 alveoli cells of the alveolar wall. The Type 2 cell are green and have a sort of different shape and sit immediately inside the surface. They secrete this material called surfactant which is very heavy in phospholipids which creates a very thin slippery film. If this surfactant wasn’t there the surfaces of the alveolar walls would stick together and it also helps keep the balloon from collapsing. You know how hard it is to blow up a balloon, so we wouldn’t want to have to deal with these sacs collapsing.
The walls of the alveolus (plural for alveoli) have these red spots. Each red spot is a single endothelial cell of a capillary. This is where exchange occurs of the gases and it’s this tiny space that makes the respiratory membrane.
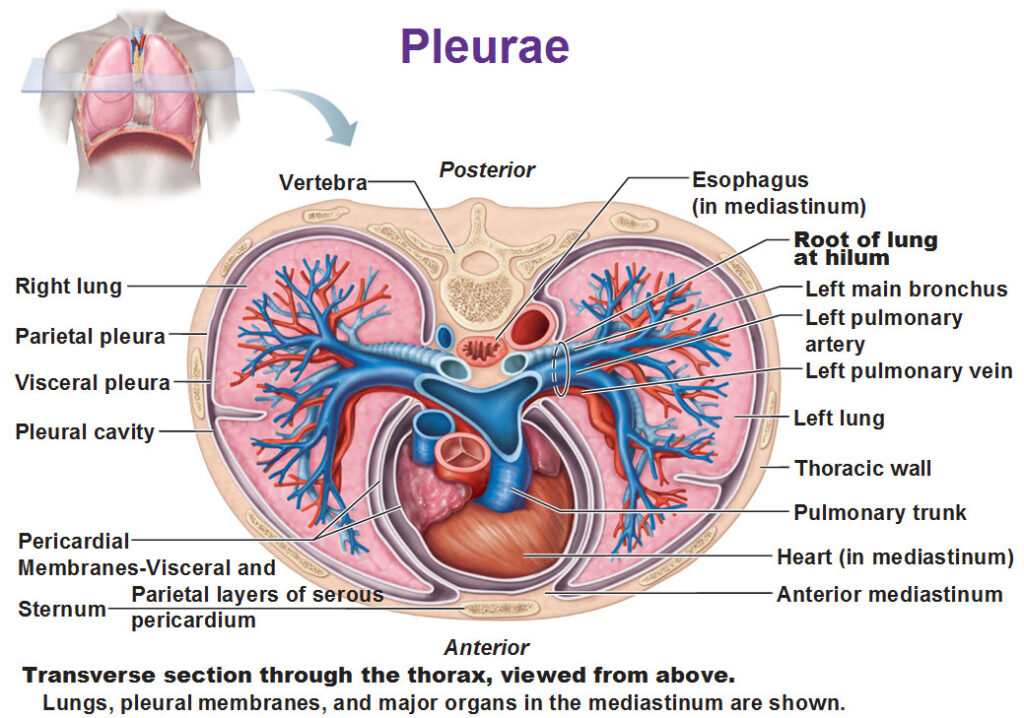
Pleurae
A pleura is a the thin covering that protects and cushions the lungs. Pleurae is plural for pleura. Here is a cross section below of the pleural cavity by looking down into the thorax. Note the heart, the left lung and right lung, the left bronchus and right bronchus. There’s blood vessels running along those branches. So that gives you an idea of the setup. And oh look at the pleural cavity, what kind of membrane is the pleural cavity surrounded by? Serous Membrane! Remember the parietal layer is what lines the cavity and the visceral layer covers organs. So in this case the visceral pleura covers the lungs while the visceral layer of the pericardial membrane covers the heart. And remember there’s a little bit of fluid in a serous membrane, so the lungs can easily glide against the rib cage.
Use this Table of Contents to go to the next article

YOU ARE HERE AT THE SPECIALIZED SYSTEMS