Inflammation and the Pathophysiology of Fever
Our first thought of fever is that when people have fevers, they may have shivers and feel chilly. What you’re going to actually learn is that your understanding is actually the reverse of the reality. Before we get into this, we need to address inflammation for any of this to make sense. The inflammatory response is a generic response no matter what is injuring the body. The purpose is to destroy noxious (harmful) agents and help the tissue heal and get better.
The Inflammatory Response (aka the Non-Specific Immune Reaction)
Injured tissue cells release chemicals that cause inflammation called “chemical mediators of inflammation.” These chemicals primarily produce their effects in the localized areas where they are released. Let’s first talk about 3 broad things that could cause cells to release chemical mediators of inflammation:
1) Microbial infections caused from things such as lytic viruses. Most viruses are lytic (called that cause they causes lysis, rupture of cells). Bacterial infections are another type of microbial infection. Flu, hepatitis, HIV, are all lytic cells that destroy/injure cells. They are eating your cells. Fungal infections exist too. If you have atheles foot, that’s eating off your skin. If your have strep throat, the bacteria is eating up your throat.
2) Trauma doesn’t necessary involve injury. Trauma could be a paper-cut. If you cut something or burned your skin from a fire or got UV radiation (sun burn), that damages the cells.
3) Exposure to allergens. What is an allergen? An innocuous (harmless) foreign agent. Some people have hypersensitivities to a harmless foreign agent, such as pollen from flowers. There’s nothing harmful about flowers but some people are hypersensitive to pollen and they will sneeze, their eyes will water and their throat will get scratchy. These people will start to release histamine and kinins, as if injury had occurred, but really nothing had occurred. Some people are allergic to foods, foods that are not problems to most people. Some people are allergic to medications, such as penicillin (about 8% of the population). In this case, there is not actual damage to the body but the body ACTS like it got damaged.
Chemical mediators of inflammation
- Histamine
- Kinins
- Leukotrines
- Prostaglandins
- Interleukin-1 (“leukocytic pyrogen”)
Interleukin-1 is the newer name for a leukocytic pyrogen (Leuken means it’s produced by red blood cells, -cytic means cell. Pyro in pyrogen means fire/fever and gen for genic/genesis/creation of.)
Prostaglandins are special in the sense that they can be carried in the blood stream to your brain where they affect the neurons in the thermoregulatory reflex center, causing fever. Prostaglandins raise the set point in your brain.
Do you remember we talked about prostaglandins when we went over lipids because prostaglandins are a type of fat? When any cell is injured or suffers trauma, it disrupts the phospholipid membrane. A chemical process converts some of these phospholipids into prostaglandins.
Characteristics of Inflammation
If you hammer a nail and accidentally slam your thumb, the thumb will get red, warm, swollen and hurt. If you have strep throat, your throat will be red, warm, swollen and hurt.
Redness and Warmth: Histamine causes local vasodilation, increasing blood flow to the injured area. Warmth and redness is created because the vessels near the injury dilate. Why? This brings more antibodies and white blood cells to the injury because they are carried by the blood vessels. Increasing the flow of blood also brings more oxygen and nutrients to the area. This explains the redness and warmth.
Swelling: These chemicals also cause capillaries to be more permeable or leaky. Capillaries are just one cell layer thick (simple squamous epithelium) and all chemicals can easily diffuse through cell walls except for proteins. Proteins in the blood stream are called plasma proteins. The only new thing this added permeability permits are these plasma proteins. As the proteins leak out of the blood vessel, they osmotically draw water with them.
Do you remember we said that people with diabetes have so much sugar in their blood stream that it spills over into their urine and that drags more water into their urine and that is why the classic symptom of diabetes is frequent urination? If not then please review the reason why ketoacidosis occurs in unmanaged diabetes due to the catabolism of fats.
Another example we already talked about: When you pour salt on a snail, doesn’t that draw water out of the cell? Water is drawn toward areas that have solute in them. Water follows solute. If you don’t remember this, please review the effect of osmosis on cells.
As the proteins flow out of the capillary and osmotically draw water with them, that’s what creates swelling or localized edema (edema means swelling). What is the purpose of these proteins coming out to the site of injury? Some of these proteins are antibodies.
Pain: Some of these chemicals, specifically the prostaglandins and kinins, activate the pain sensory neurons. What good is pain? It warns you that something is wrong. Two quick examples: If you step on a piece of glass and you’re barefoot. If it didn’t hurt, you’d keep walking, driving that piece of glass deeper in your foot. If you’re playing with bare wires and got electrocuted and it didn’t hurt, you’d keep playing with it until you die of electrocution. In some ways it’s unfortunate that cancer does not cause pain sooner because commonly when someone feels pain from cancer the cancer has spread too much.
Chemotaxis: Some of the chemicals released by injured cells release white blood cells (neutrophils are small phagocytes and monocytes are macrophages; Macrophages are king of the phagocytes) to the injured tissue and this is called chemotaxis. Chemotaxis means a movement (taxi) in the direction of where chemicals (chemo-) are coming from. White blood cells are attracted toward the infected or injured areas because of chemicals. These chemicals attract WBC’s to phagocytize the bacteria and also the dead human cells because the place needs to be cleaned up before healing occurs.
Fever: Chemicals are being released from injured cells, carried from the blood stream into your brain and raising the thermostatic set point to a higher level. If you have your thermostat in your home raised from 70 to 80 to 85. That will cause the heater to turn on until it reaches that new higher set point. Leukocytic pyrogen and prostaglandins act on the hypothalamic neurons, the thermostatic center of your brain, causing an increase in the thermostat set-point.
The classical febrile response (Fever!)
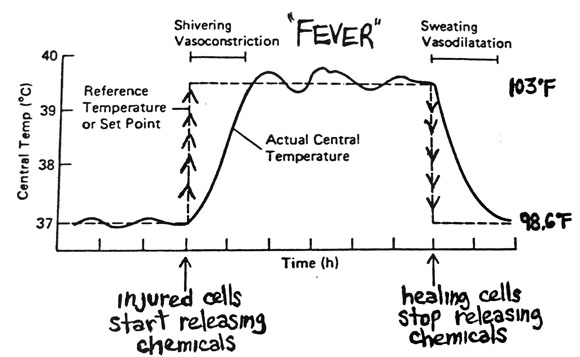
Below you see a graph with the X-axis being time and the Y-axis as temperature. This graph shows two lines. A dashed line and a solid line. The dashed line starts out at 37°C (98.6°F) and that’s the set point. We said your actual body temperature oscillates around that because your body doesn’t activate heating or cooling mechanisms until the temp goes below or above the set point, respectively.
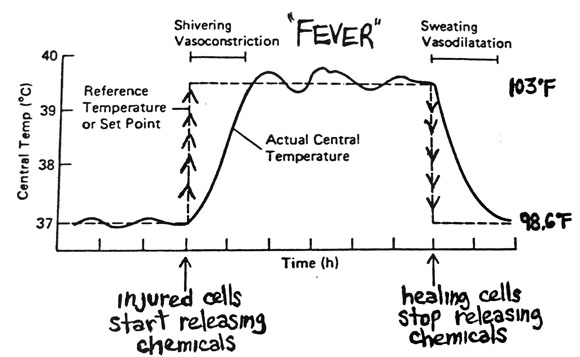
The onset of fever
We said interleukins and prostaglandins raise the set point. It’s generally believed that the greater the injury, the more of these chemicals are released and the greater the set point is raised. In other words, the higher the temperature is raised, the greater the injury is. So let’s say your new set point is now 103°F and your actual body temp is 98.6°F and the Thermoregulatory Reflex Center COMPARES the two and thinks you are way colder than you should be! So what happens next? The control center is going to tell the body to warm your body up to 103°F!
Injured tissue cells release chemicals -> increase in temp set point -> activation of “heat generating mechanisms”
Let’s review the homeostatic reflexes that are activated whenever the body temperature is LOWER than the set point: You will feel cold, blood vessels in your skin constrict (you look pale), and you start shivering. If you’re lying under a bunch of blankets and you’re shivering, you’re going to get really hot. The shivering and blankets are going to make your temperature sky rocket.
The breaking of the fever
healing tissue cells stop releasing chemicals -> set-point returns to normal -> activation of “cooling mechanisms”
Let’s suppose there’s a viral infection so it’s totally up to your own immune system to fight it because we don’t have antiviral drugs that do anything. There’s a wisdom to the body that allows us to survive these things. Either the virus kills you and the story ends there, such as with elderly with weak immune systems. Or, the cells starts start to heal and stop releasing the chemicals that cause fever (prostaglandins and the interleukins), returning back to the normal set point but now, your actual body temperature is at 103°F. Now what will happen?
This will activate the homestostatic reflexes for cooling: You will feel very hot (kick the blankets off), your blood vessels in your skin will dilate (you’ll get red) and you’ll start to sweat (some people will sweat so much they will soak their sheets). This is known as the “breaking” of the fever because the set point will return back to normal.
Is the fever beneficial?
Remember this is being caused by the chemicals produced by your own cells, at least in part. Recent studies have shown that a fever raising the body temperature enhances the immune response, increases the production WBCs and interferon proteins, and the fever may slow down the multiplication of some pathogens (like say, bacteria). Bacteria grow in an optimal pH and temperature range. Many of the worse bacteria that causes us to get sick such as colds, flu and pneumonia are in our lungs. The lungs are the coolest part of our body. Why? Because every time we exhale, we lose heat. Your intestine is the warmest part. The bacteria that thrive in our body like to live in our lungs because it’s cooler. Raising our body temperature higher than normal in our lungs, raises it higher than preferred for those bacteria.
We know that high body temperatures are dangerous due to the potential denaturation of proteins leading to coma and then to death. If your fever is 101°F though, that’s not a big deal. If you’re exercising in a hot temperature, your generating lots of heat and your body temp is probably 100-101°F anyway. A low grade fever that’s 101°F or less is not life threatening. If it’s a high-grade fever (more than 101 degrees), then cooling needs to occur, but it’s really, really, really rare an adult is going to run a really high fever, like 105 or 107. The only people that develop these scary high fevers are infants. Infants brains are not fully matured and their thermoregulatory reflex center are not fully normal yet. However, as adults, it’s very unusual that this occurs.
How does Aspirin work as an anti-pyretic agent?
Aspirin, like most drugs, have many actions and many uses. Aspirin is described as an anti-pyretic (pyrogen causes a fire or fever). You’ll also see aspirin described as an analgesic (algia means pain). Aspirin is also described as an anti-inflammatory drug (NSAID). Aspirin can even be used as a blood-thinner.
Aspirin was originally obtained from the bark of a willow tree. In the late 1800’s, Beyer isolated the active chemical. Nowadays there are variations called acetaminophen (Tylenol) and ibuprofen (Advil) and naproxen (Aleve). They only discovered how aspirin works in the 1970’s and the people (Sune Bergstrom and Bengt Samuellson of Stockhold University) were awarded a Nobel prize for it. They work by stopping the synthesis and release of prostaglandins. They are prostaglandin inhibitors.
If you have a fever and you take aspirin, it lowers your fever, but what if you don’t have a fever or injury and you have a normal body temperature and you take aspirin? Will aspirin lower your body temperature? No. It stops prostaglandins from being released. If you’re not releasing prostaglandins then it will have no affect. We will have a little more talk about this next time.
Why would you want to stop inflammation?
If the inflammatory response is supposed to be beneficial in general and pain is supposed to warn us of something being wrong, then is it really a good idea to take tylenol to reduce that? If your fever is not too high, then it’s part of the healing response and it’s probably not a good idea to take drugs. The doctor would say drink plenty of fluids and get lots of rest. If you keep egging the doctor on to prescribe something for you so your visit won’t feel like a waste, then the doctor would say take tylenol but there’s nothing we could do against fighting viruses if you have a cold or flu. Even if you have a bacterial infection, the tylenol won’t help fight that either. All tylenol does is reduce the symptoms and it’s probably delaying the healing process but we take it because plain and simple, we don’t like pain.
Chronic inflammation, however, that isn’t helping the body anymore is bad for the body. Arthritis, for example, or more specifically rheumathoid arthritis, involves not only chronic inflammation but also WBC’s that are also attacking the body. Phospholipase is what eats up disturbed cell walls (and turns phospholipids into prostaglandins). Steroidal Anti-Inflammatory drugs (not NSAID’s) such as cortisone and prednisone stop phospholipase. If phospholipase is stopped, none of the histamines/hormones are released. So if you use a steroidal anti-inflammatory drug, it will stop ALL these things.
Basic Physiology Primers
- The Concept of a Reference Person
- Review of Cell Membrane Structure
- The Proteins Embedded in Cell Membranes
- Fluid Compartments within the Human Body
- Movement of substances across cell membranes
- The Principle of Homeostasis
- Regulation of Body Temperature
- Inflammation and the Pathophysiology of Fever (YOU ARE HERE!)
- The Menstrual Cycle






