The Renin Angiotensin Aldosterone Reflex
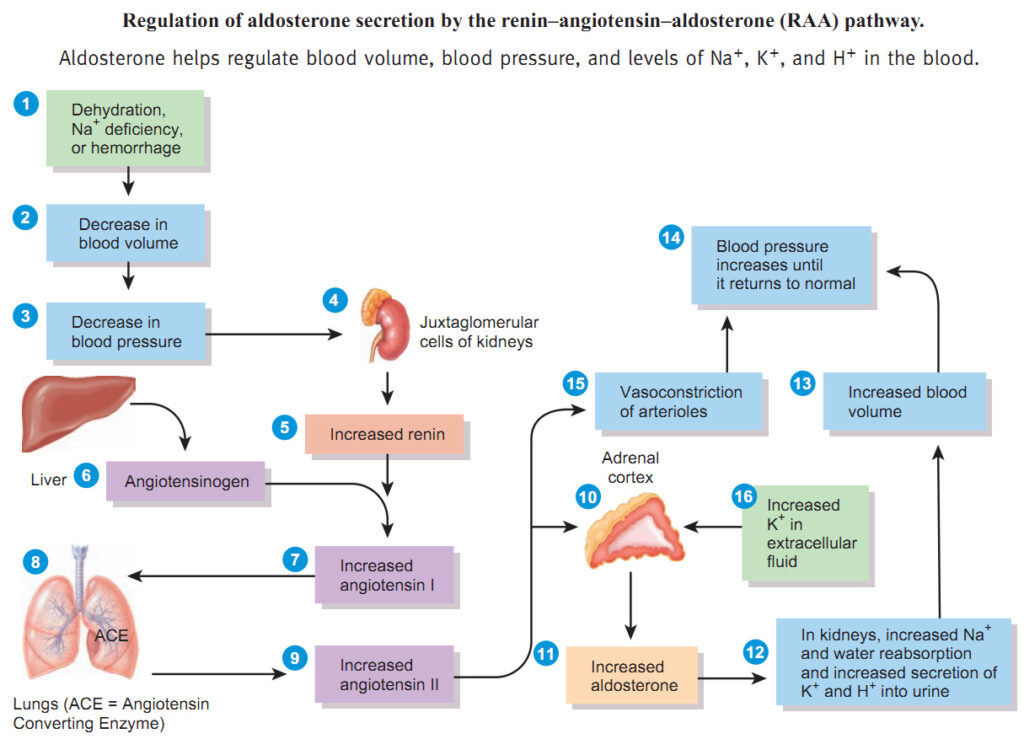
We are going to talk about the homeostatic reflex mentioned as the following things in a textbook:
- renin-angiotensin system (RAS)
- renin-angiotensin-aldosterone system (RAAS)
- renin-angiotensin-aldosterone pathway (RAA pathway)
Don’t let these words scare you! We’re going to follow a pattern here. Renin leads to Angiotensin being released which eventually leads to Aldosterone being released. We’re going to explain all that in detail.
We begin with the kidney. The kidney is an endocrine gland (since it secretes several hormones) and it excretes two hormones we are going to learn about: renin (renal means kidney) and erythropoietin (brand name Procrit). The cells that secrete renin are called Juxtaglomerular (J-G) cells.
Three triggers that cause JG cells to secrete Renin into the blood stream:
- A drop in blood pressure,
- A decrease in blood sodium levels,
- An increase in blood potassium levels.
That triggers this hormonal homeostatic reflex. A homeostatic reflex is there to compensate or correct for a stress.
Examples of homeostatic reflexes:
- If you’re too hot, the homeostatic reflex is to sweat to cool yourself down.
- If you walk into a dark room, your pupils dilate to take in more light.
- If your blood sugar is too low, you release hormones that raise your blood sugar level.
The RAA pathway ensures that it will correct for all three of these triggers. It makes this a very important reflex because it controls your blood pressure and your two most important minerals in your body: sodium and potassium.
When Renin is secreted, it stimulates a protein in your blood stream called angiotensinogen. The liver makes most of these plasma proteins (such as albumin). This angiotensinogen is always circulating in the blood stream. Renin activates it and turns it into angiotensin-1.
(There are many proteins that have to be “activated.” The inactivated form usually it ends with -gen. Then when it’s activated, you drop that ending so it becomes angiotensinogen to angiotensin 1. For example: Your stomach cells secrete something called pepsinogen and the hydrochloric acid activates it into pepsin. During blood clotting, Fibrinogen is turned into fibrin.)
How does Renin activate Angiotensin?
Angiotensinogen is a polypeptide. Renin cleaves four of the last amino acids in the molecule, and changes it to Angiotensin I, so to say it got activated, was to mean it got shorter.
There’s an enzyme in your lungs called ACE which stands for Angiotensin Converting Enzyme and as Angiotensin-1 is carried to your blood stream to your lungs, it becomes Angiotensin-2. ACE basically cleaves off the last 2 amino acids of Angiotensin-I, making it an even shorter polypeptide chain and that is Angiotensin-2 now. So it’s been cleaved/spliced twice so far.
Angiotensin-2 is now in the blood stream and it specifically activates the adrenal cortex to secrete aldosterone and other mineralcorticosteroids. Remember the adrenal cortex secretes: adrenoandrogen, glucocorticosteroids and mineralcorticosteroids.
- What controls the release of glucocorticosteroids like cortisol is ACTH.
- What controls the release of aldosterone and other mineralcorticosteroids is this RAAS.
This aldosterone that is released from the adrenal cortex (due to the angiotensin-2) will affect the kidneys.
Aldosterone will make the kidneys do three things:
- Increases Potassium excretion; Potassium in the blood stream is excreted into the urine (to be eliminated). That compensates for when your blood potassium level is too high (one of the 3 original triggers!). When the K+ is too high, the RAA system causes the potassium to be excreted out. Remember when we talked about Hyperkalemia we said the reason there’s no warning label on every Chiquita banana for its potassium content because your kidneys will excrete it out.
- Increase salt retention: It causes your kidneys to retain salt and compensate for low sodium levels. Instead of kidneys peeing out that salt, you retain it.
- Increase water retention which together with the increased salt retention, that causes your blood pressure to increase in your vessels. This is not like ADH. ADH causes you to retain ONLY water to dilute the salt. Here you retain both salt and water, so you are retaining isotonic fluid. The purpose of this is to expand your blood volume and by doing that, that raises your blood pressure, and that compensates for what initiated this reflex (a drop in blood pressure). If you have a cut and you’re losing blood, your blood pressure will drop. If you increase the amount of water and salt retention, you will increase the blood pressure. How cool is that?
The Aldosterone will raise the BP, raise Na+, decrease K+ because it causes the kidney to retain salt and water. People always confuse this with Anti-Diuretic Hormone (ADH), so make sure you don’t. 🙂
What’s the difference between ADH and Aldosterone?
If you eat food that’s high in salts, you increase the tonicity of your bloodstream when it’s absorbed and become hypertonic. That triggers ADH which causes your kidneys to retain water and only water. A drop in blood pressure will also cause ADH release because there’s a multiplicity to the body all the time.
There’s never been a clinical case of somebody overproducing ADH. But there are clinical cases of lower than normal ADH levels (deficiency) which goes by the name of diabetes insipidus. What’s diabetes insipidus? If you can’t make ADH, you pee a lot because you have no way of not-peeing a lot. The word diabetes means to pee a lot. There’s diabetes mellitus. Mellitus means sweet. So this is sweet pee. Insipidus is pee that doesn’t taste sweet. These two diabetes were recognized by ancient greeks. When people would pee a lot, they would taste their urine. If it tastes sweet, it was called diabetes mellitus, and if it wasn’t sweet it was called diabetes insipidus.
With diabetes mellitus, you don’t have enough insulin so it leads to hyperglycemia which spills into the urine (glycosuria, tested by dipstick), and it osmotically draws water (osmotic diuresis) with it, so people with diabetes pee a lot. Review ketoacidosis in unmanaged diabetes section.
Here’s a chart below to help you note the differences.
On the right is aldosterone which increases both salt and water retention and increases potassium secretion… it regulates your Na+K+ and blood volume.
| Anti-Diuretic Hormone (ADH; Vasopressin) | Aldosterone | |
|---|---|---|
| Source of Hormone | produced by hypothalamic neurons; stored and secreted from the Pituitary Gland (neurohypophysis) | secreted by the Adrenal Cortex |
| Factors that lead to the release of the Hormone | ↑ Osmolarity (tonicity) of CSF. ↓ Systemic arterial BP |
↓ Renal Blood Pressure (1) ↓ Plasma [Na+] (2) ↑ Plasma [K+] (3) [-> Renin -> Angiotensin] |
| Action of Hormone | ↑ permeability of urine collecting ducts to H2O Small volume of concentrated urine. |
stimulates Na+/K+-ATP pumps in the distal convoluted tubule portions of the nephrons -> Small Volume of Isotonic Urine |
| Function of Hormone | ↑ H2O retention Maintenance of Plasma Osmolarity (Tonicity) |
↑ NaCl and H2O reabsorption ↑ K+ excretion Maintenance of Plasma Na+ and K+ electrolyte levels |
| Syndrome Associate with Hormone Excess | (not clinically reported) | Hyperaldosteronism ↑ NaCl retention (hypernatremia) ↑ H2O retention (hypervolemia; + blood volume; renal hypertension) ↑ K+ excretion (hypokalemia and hyperpolarization; slowing down) |
| Syndrome Associated with Hormone Deficiency | Diabetes insipidus. Production of large volumes of isotonic (or even hypotonic) urine. |
Hypoaldosteronism ↓ NaCl retention (hyponatremia) ↓ H2O retention (hypovolemia; – decreased blood volume; circulatory shock) ↑ K+ retention (hyperkalemia and depolarization;speeding up) |
Hyperaldosteronism: At the lower right, we talk about too much aldosterone. It causes a rise in the blood pressure, called renal hypertension because you’re retaining salt and water which leads to hypervolemia, hypernaremia and hypokalemia. This is a problem but not fatal.
Hypoaldosteronism: A deficiency in aldosterone is fatal because you don’t retain salt or water and don’t excrete potassium which leads to hyponatremia, hypovalemia and hyperkalemia which leads to depolarization of all the cells in the body, which causes increased activity of your muscle cells and what kills you is eventually the fibrillation of the heart. By retaining less volume and salt, your blood volume drops and your blood pressure drops and this is circulatory shock.
Since we mentioned renal hypertension as a cause of hyperaldosteronism, let’s go over hypertension.






